Hello, everyone! I’m sitting at my desk again. It’s been a while since I’ve written anything. I took some time off to deal with a pretty hefty health issue. Still dealing to be honest, but on the upswing. I’ve learned it’s hard to focus on writing while dealing with the stress of a bad illness and the fatigue that comes with it.
So, what was wrong with me? Last summer, I was diagnosed with a leaky heart valve after I almost passed out one day. I’d had shortness of breath, which I attributed to my anemia that I’ve had for a while now. The valve issue seemed manageable with medication for about eight months and even cleared up my shortness of breath issue some.

Image: Heart diagram with examples of healthy and stenotic aortic valve. source: Longmore Clinic
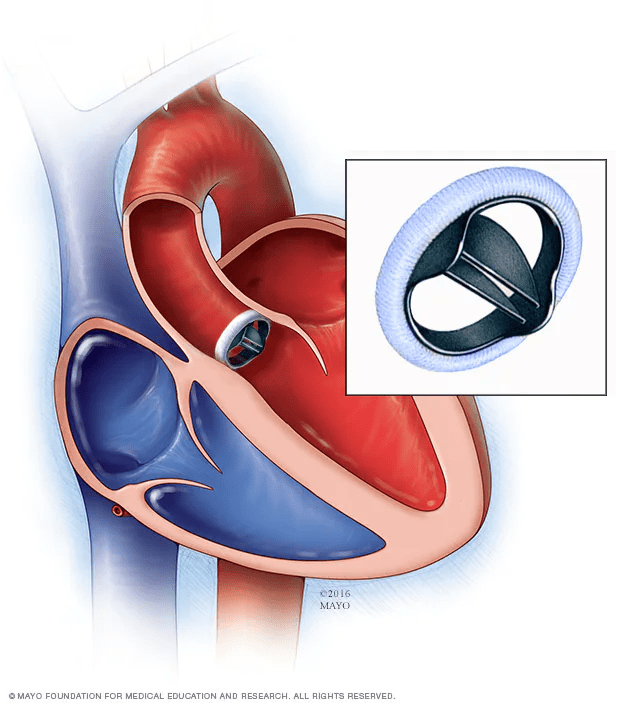
Image: Diagram of the heath with a mechanical aortic valve. source: Mayo Clinic
To make matters worse, I found a small lump. It was sitting between my skin and my breast implant, in almost the exact same position as the last tumor. I went back to Mayo and got the fast-track treatment because that wasn’t supposed to happen. The lump was removed in September, and I had 15 rounds of radiation in December. My ovaries are also medically shut down for the next five years or so. I’d like to say I’m cancer-free again, but now I’m guarded about such a declaration. We’ll see how that goes over time. Back to my heart.
In March, I had trouble breathing and went into the ER again. My valve was worse (from ‘mild’ to ‘moderate to severe’ regurgitation was the terminology) and I began losing energy with even small exertions. I had a TEE done. That’s a transesophageal echocardiogram for all of us that had no idea. They do an echo of your heart from inside your esophagus…while you’re awake. Fun times. The esophagus is right next to the heart, so it gives the doctor a much better view of the heart structure. My valve was bad. I could hear him whisper to the ultrasound tech that I needed a new valve. I didn’t ask questions. I couldn’t. The probe was still down my throat.
A few days later, I was in my cardiologist’s office hearing that same news. My valve was far worse than before and my heart was working overtime to keep up, a recipe for heart failure. I needed to have the replacement done within six months. So, I started the process of finding a surgeon. I tried to go back to Mayo Clinic, but the process seemed to take forever. I wanted this done as soon as possible. To be fair to them, I probably would have had the surgery around the same time, but I was able to secure the scheduled time faster with a surgeon who worked at St. Joseph’s hospital in Phoenix. I had worked there and was confident in their doctors and staff. It helps your confidence when you see the doctors work on other people. Luckily, though, he also did cases at Chandler Regional Hospital (same hospital system, Dignity Health), which is much closer to home, and I had my surgery there.
I was scheduled for surgery on June 19th. Perfect because my mom’s birthday was the 18th, and we could take her to a nice dinner beforehand. Well, on the 17th, they called me and asked me to move up to the 18th. That was fine, but I had to move reservations around. We had a great dinner at Elliott’s Steakhouse in downtown Chandler. My sister was also in town, so it was an awesome evening.
I was mentally well prepared for the procedure, but it was the most nerve-wracking wait I’ve ever had before going under the knife. When I got in the room, the nurse introduced me to everyone, the last being the perfusionist that would run the bypass machine. Bypass, to me, is a magical process. They shut down your heart and lungs. Your blood runs through a machine that oxygenates the blood and returns it to the body. That part isn’t magical to me. I get the science of it. The last step holds the magic. That’s when they jump start the heart and lungs and get you going again. It’s rather amazing to me that those organs can be shut down for hours and then start again like nothing happened (almost). I’ve even been in an OR and watched the process happen, and I still can’t wrap my head around it. That it happened to me still bounces around in my head as a surprise sometimes.

Image: A cardiopulmonary bypass machine in use during surgery. source: The Physiological Society
Looking at the machine is the last thing I remember before waking up in the ICU. Technically, I woke up three or four times in the ICU that night. The first time, I had the dazed “where am I?” thoughts for a few moments before I remembered. Then, I felt the tube in my throat and hoped I wouldn’t gag right before I did. I could hear people around me, telling me not to pull the tube out of my throat. I wasn’t planning on it, but I imagine I wasn’t fully running the Sarah show at that point. I tried to give a thumbs up to show I heard them. I have no idea if I was successful. I think I opened my eyes a tiny bit because I remember seeing a nurse pushing propofol into my IV. I may also have been making that part up. I did fall back to sleep right after. The process repeated one or two more times before I was breathing well enough to pull the tube out.
They kept an eye on me as I woke up. Once they deemed my heart and lungs ready (within a day I think, this part is fuzzy), they transferred me to the cardiac ward for the rest of my stay.
There, I ate, slept, got meds, and started getting out of bed. At first, there were just trips to the bathroom, but they quickly started making me walk in the halls. Walking was hard work. My lungs were not fully inflated yet. That’s how I describe the sensation at least. When they would listen with a stethoscope and tell me to take a deep breath, all I could do was a tiny gasp. As the days passed, the gasp got bigger and bigger. They gave me an incentive spirometer to help build my lung capacity back up. By the last day, I could breathe comfortably, but still had a ways to go for a full breath.
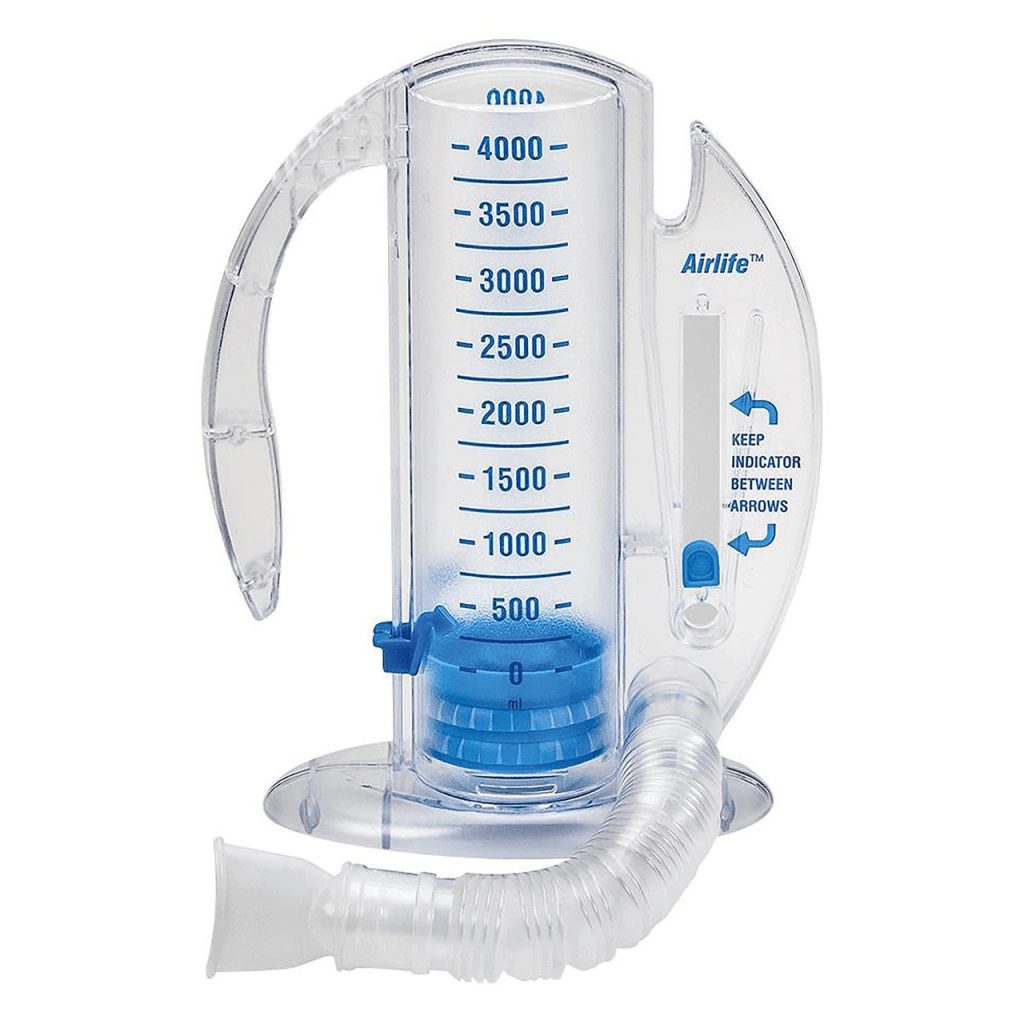
Image: Photo of an incentive spirometer. source: Beyond Surgical Supply
People came to see me. My sister came for the first couple of days until she had to go home. My mom and husband came every day and sat with me. A couple of good friends from grad school dropped in for a while. It was nice to see them all, but I was not the best company then. I guess that’s to be expected.
Surgery was on a Tuesday. I went home on Sunday. My tubes and lines were all removed. I got a huge pile of instructions. There were a ton of appointments to make. It all sounded exhausting, but I managed to get it all done over the next few weeks.
Home PT was actually kind of fun. The therapist was very nice and eased me into the routine. Mom did my PT with me on the days the therapist didn’t come. There were a lot of light leg exercises for strength, balance, and stamina.
I weaned off the pain killers.
At six weeks post-surgery, I was able to drive again. I took it slow but didn’t have any issues. Then it was time to say bye to mom. She had been so helpful during her stay, but we all had to get back to normal. Dad missed her, too. In the meantime, school has started. I’ve begun cardiac rehab, which is more cardio exercises to build up my heart while being monitored by a nurse and physical therapist. I go three days a week until sometime in October.
I’m feeling better than I have in a long time. I feel ready to accomplish more of the projects I’ve planned on around the house. I’ve been cleaning up a lot of the clutter that’s accumulated with a lot more to go. It’s exciting to get life back in order.
The funniest comment I received throughout this process was how good I looked at every stage. After a little while, I realized why. I’m 45 years old and most people receiving a new valve are at least 20 years older. The procedure takes a lot out of you and recovery can be very difficult. There is a big difference in those 20 years when talking about how well one can recover.
I am motivated to regain a lot of what my life once was and more if possible. I believe this valve issue has been impacting my life for a very long time but either wasn’t detectable or wasn’t causing bad enough symptoms to trigger a doctor to look. Because of that, I have a sort-of goal that I want to test out. I want to know if I can run now. It’s been decades since I could run much at all because I would lose my breath. I was even diagnosed with sports-induced asthma, but the inhalers never helped, but I wonder if my heart valve was causing issues as far back as my teens. It’s a sort-of goal because I don’t have the expectation that I’ll accomplish it. It’s more of a hypothesis that I’m testing. It will be awesome if I can run. A jog in the mornings would be a nice way to start the day.
My next big goal is to start writing regularly again. I received some very helpful and positive feedback regarding my book from a publisher and will tackle those changes soon. I’m also planning a Kindle Vella project and want to write more in this blog. I’m still reading Stephen King in order and need to catch up on those posts, but also I have some topics I want to explore.
Anyway, that’s been my life this summer and I’m excited to get back to it.
Quick edit to add a shoutout to Edward Bauman on Youtube for posting a video about his experiences with his mechanical aortic valve replacement. I felt so much more at ease though the process because I knew what to expect from his video. https://www.youtube.com/watch?v=r4vOu5bzHLk
